Understanding Type 2 Diabetes
Causes, Symptoms, and Management
What is Type 2 Diabetes?
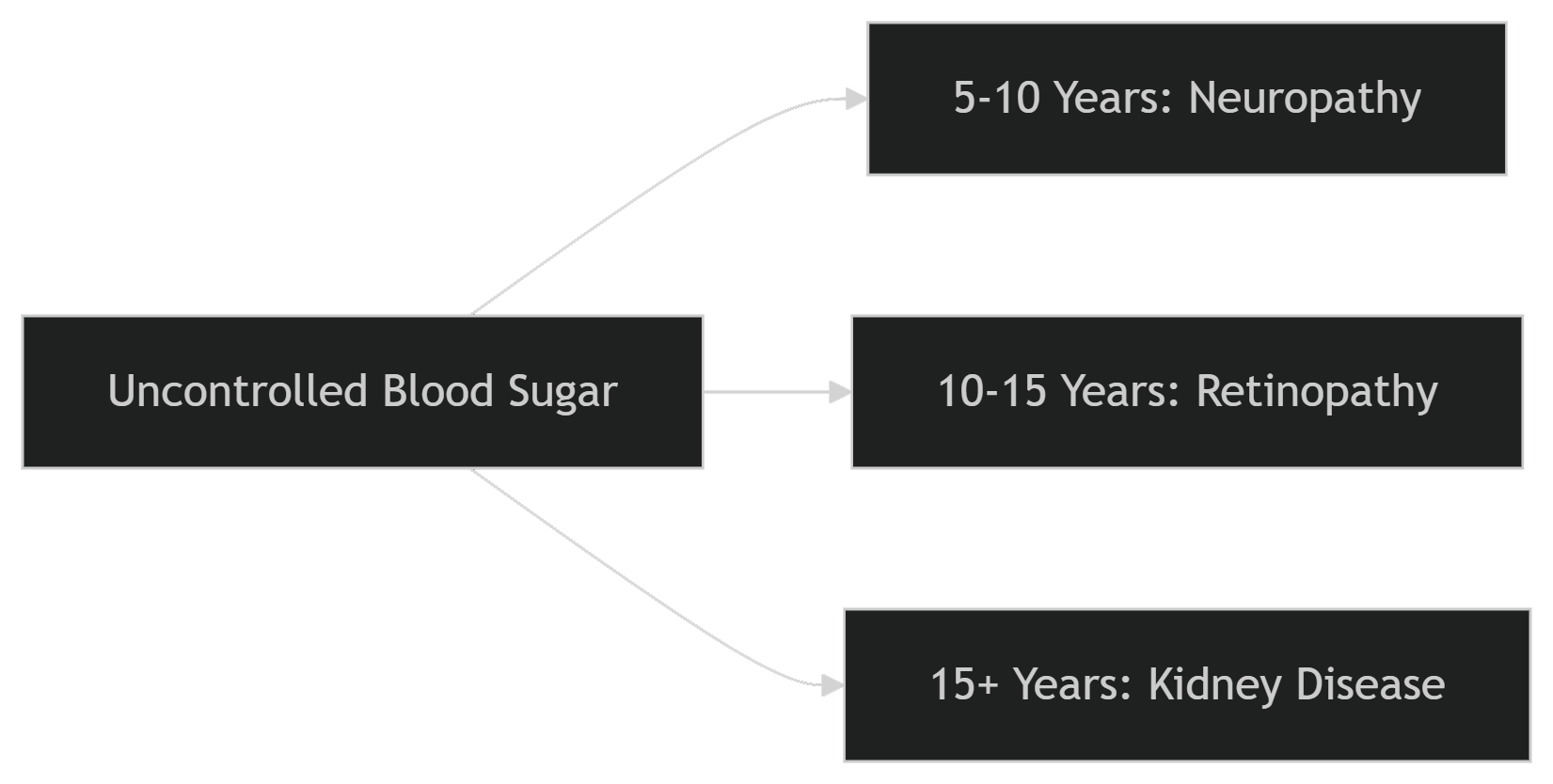
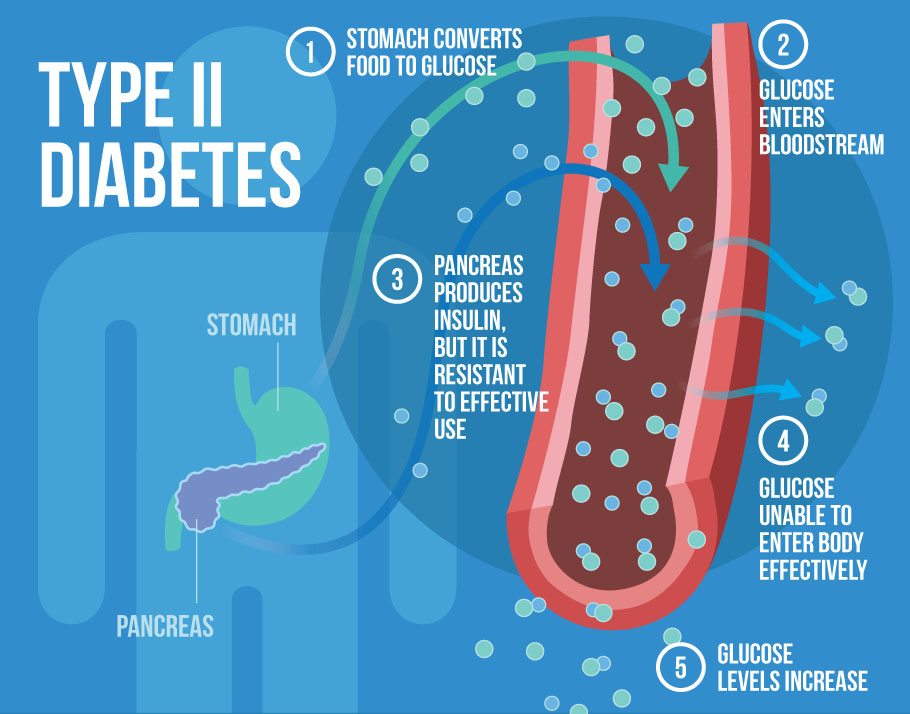
Type 2 diabetes is a chronic metabolic disorder where the body becomes resistant to insulin or doesn't produce enough insulin, leading to elevated blood sugar levels. Unlike Type 1 diabetes (an autoimmune condition), Type 2 is often linked to lifestyle factors and develops gradually.
Key Symptoms to Watch For
Increased thirst and frequent urination
- Excess glucose pulls fluid from tissues, causing dehydration.
Fatigue
- Cells deprived of glucose energy.
Blurred vision
- High blood sugar affects eye lenses.
Slow-healing wounds
- Poor circulation and nerve damage.
Tingling in hands/feet
- Early sign of neuropathy.
Root Causes and Risk Factors
| Risk Factor | Explanation |
|---|---|
| Obesity | Fat cells release inflammatory chemicals causing insulin resistance. |
| Sedentary Lifestyle | Activity helps muscles use glucose effectively. |
| Genetics | Family history increases risk by 40-70%. |
| Age | Risk rises after 45 due to reduced insulin sensitivity. |
| Gestational Diabetes | Increases lifetime risk to 50%. |
Evidence-Based Management Strategies
Diet and Nutrition
Dietary Approaches
- Low-glycemic foods: Beans, non-starchy veggies, berries
- Healthy fats: Avocados, nuts, olive oil
- Protein balance: Fish, poultry, tofu
Sample Meal Plan: Breakfast: Greek yogurt + chia seeds + blueberries Lunch: Grilled salmon + quinoa + roasted Brussels sprouts Dinner: Turkey chili with kidney beans
Exercise Recommendations
- 150 mins/week of moderate activity (brisk walking, swimming)
- Resistance training 2x/week to improve glucose uptake
Medical Interventions
- Monitoring: Target A1C <7% for most adults